Your heart’s job is to keep your pulse steady to pump blood throughout your body. Sometimes your heart rate is slower when you’re relaxing, and sometimes it’s faster when you’re exercising or stressed. If your heart’s ability to keep the beat
Your heart’s job is to keep your pulse steady to pump blood throughout your body. Sometimes your heart rate is slower when you’re relaxing, and sometimes it’s faster when you’re exercising or stressed. If your heart’s ability to keep the beat starts to go awry, cardiac electrophysiologists like me[1] look for outside help from an implantable device.
There are two common implantable devices for the heart: artificial pacemakers[2] and defibrillators[3]. Artificial pacemakers keep blood and oxygen flowing during times of stress. Defibrillators are devices that detect dangerously fast heart rates and deliver shocks like those used during cardiopulmonary resuscitation, also known as CPR, to restart the heart.
Understanding how these devices work requires appreciating how the heart’s electrical system works and the weak links that cause malfunctions.
The heart’s natural pacemaker system
Abnormally slow heart rates result from breakdowns in two principal areas of the heart.
First, the sinoatrial, or SA, node[4] sets your “resting” heart rate, usually somewhere between 60 and 100 beats per minute. This is the base effort needed to circulate enough blood to sustain normal bodily function. Elevated levels of certain hormones circulating in the body, such as adrenaline and serotonin, can increase heart rate above resting levels[5].
Trained athletes frequently have a lower resting heart rate due to extra physical conditioning. Like any other muscle, the heart becomes stronger with training. Because their heart functions more efficiently, athletes require fewer heart beats overall[6] to circulate blood.
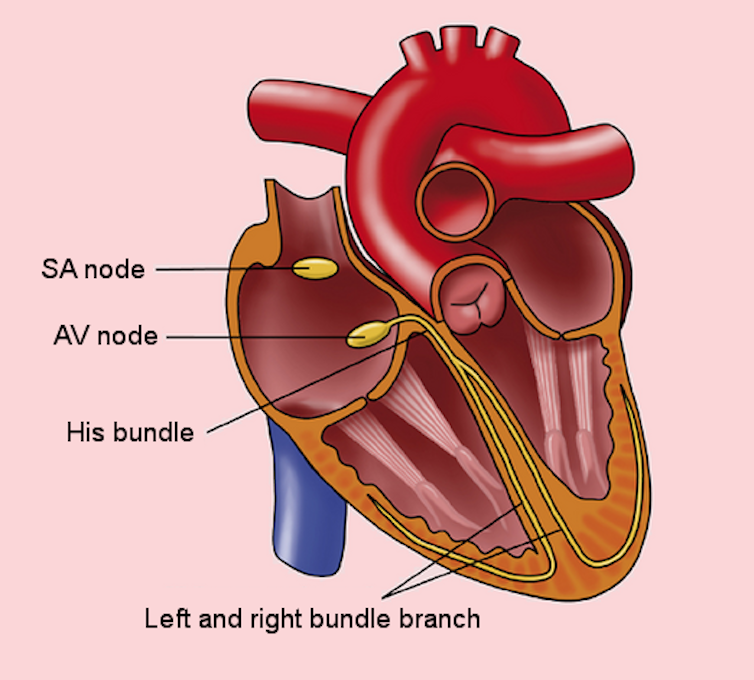
The atrioventricular, or AV, node[9] is the second key area of the heart’s electrical wiring. The atrioventricular node takes information about how fast the heart is beating from the sinoatrial node and relays it to the ventricles, the muscular portions of the heart that allow it to pump blood to the rest of the body.
When the atrioventricular node breaks down, the ventricles don’t receive the electrical signal from the sinoatrial node instructing them to “pump,” or create a heartbeat. This causes heart rate to become dangerously slow.
When heart rate is too slow
If resting heart rate is abnormally low or fails to increase with hormonal changes, pacemakers can help keep blood and oxygen circulating at a healthy rate.
Both the SA node and the AV node naturally slow with age[10], but sometimes this happens at an accelerated pace and leads to abnormally slow heart rates. Slow heart rates can also be caused by other diseases, including thyroid problems[11] and Lyme disease[12]. In these cases, slow rates are treatable without a pacemaker.
A common pacemaker system[13] has a battery and two wires that can send and receive electrical signals. One wire rests near the sinoatrial node, and the second in one of the heart’s ventricles.
If the wire near the sinoatrial node doesn’t detect any electrical activity over a set time, the pacemaker’s battery will send an impulse to the ventricle to initiate an electrical signal. Within fractions of a second, the wire in the ventricle should detect that electrical activity. If an impulse is detected, this signifies that the AV node conducted the signal correctly to the rest of the heart, and the pacemaker does not activate. If the wire doesn’t receive this signal, the battery delivers an impulse through the wire directly to the ventricle, causing the muscle to contract and initiate a heartbeat.
The heart’s muscle will only contract in response to a pacemaker impulse if the muscle is otherwise healthy. Pacemakers do not keep patients alive[14] if the heart shuts down, such as during a massive infection, blood clot or kidney failure. Pacemakers simply keep the heart rate in a comfortable range if the primary problem in the heart is electrical.
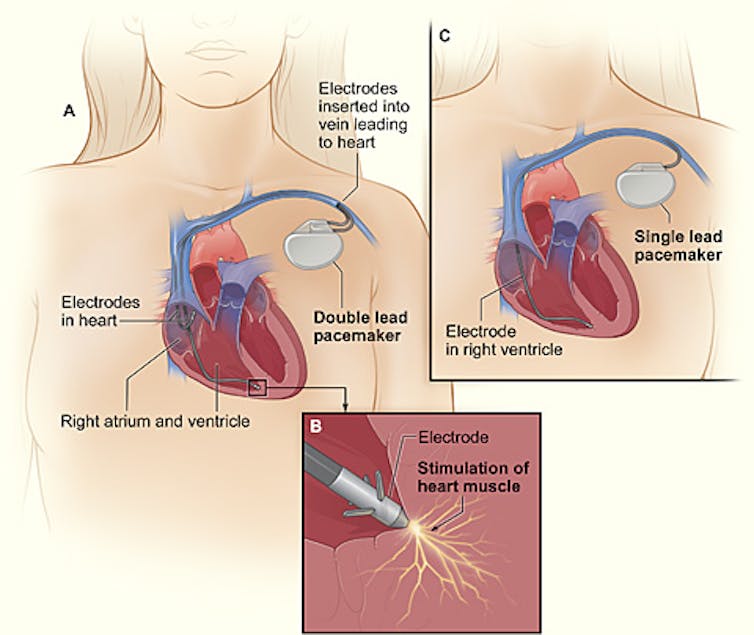
Doctors program a pacemaker’s software so the resting pulse doesn’t drop below a certain rate, commonly 50 to 60 beats per minute. If the resting rate is set at 60 beats per minute, the pacemaker will wait exactly one second before initiating an electrical pulse. The heart’s pulse rate can be higher than this number if the sinoatrial node initiates a heartbeat naturally. If the pacemaker detects activity from the sinoatrial node, it will reset its timer for another full second.
Modern pacemakers also contain sensors to predict whether the heart may benefit from a faster heart rate under certain circumstances. For example, pacemaker batteries contain accelerometers[16] like those used in pedometers to detect if a person is in motion. If these sensors activate, the pacemaker can raise its minimum rate like how the heart would normally respond to exercise. Sensors can also detect if a person begins to breathe more quickly or if the heart begins to contract more powerfully, all signs normally associated with increases in heart rate.
When heart rate is too fast
Like pacemakers, a cardiac defibrillator[17] comes with a battery and wires that record the heart’s rate. But instead of treating slow heart rates, defibrillators are programmed to detect fast heart rates, usually in the range of 200 beats per minute. Heart rates in this range are often caused by ventricular tachycardia[18] or ventricular fibrillation[19], which are potentially lethal heart rhythms resulting from the lower chamber of the heart beating too quickly or quivering.
Certain people are at elevated risk for these types of rhythm disturbances. Many cases of “sudden death”[20] in athletes and other young people are either suspected or proved to be related to ventricular fibrillation.
Defibrillators deliver internal shocks to the heart when their sensors detect either ventricular tachycardia or ventricular fibrillation. These shocks stop the heart for a fraction of a second to give the sinoatrial node a chance to resume its normal activity. These shocks can be painful[21], so doctors usually also prescribe medications or other procedures to help prevent needing the shocks in the first place.
A defibrillator is like a seatbelt: It is reassuring to have, but ideally it never needs to be deployed.
Beyond the surgery
Pacemakers and defibrillators do require some maintenance. Certain settings, such as how low the pacemaker will allow the pulse to go, can be adjusted over time[22]. Doctors have computers that can communicate with the devices and alter their programming. Some devices use Bluetooth technology.
The battery cannot be recharged and must be replaced, generally after six to 10 years. Battery life[23] depends on how frequently the heart requires the pacemaker to initiate heartbeats. Pacemaker wires[24] occasionally need to be replaced if they fracture or if the insulation wears down after years of bending with each heartbeat. On rare occasions, pacemaker parts are recalled. Usually these parts do not require replacement but may require special attention[25]. More frequent checkups of the electrical “health” of the devices are usually prescribed for early detection of any problems with battery life or wire failures.
Pacemakers and defibrillators are always changing, in part to keep up with medical and nonmedical technologies.
With cloud-based management systems that make medical information available to doctors in real time, security has become a major focus[26] of modern pacemaker software. Other medical technologies such as MRIs can change how pacemakers and defibrillators work if not handled carefully – MRIs create electromagnetic impulses that cardiac devices can misinterpret as heartbeats[27]. Modern devices are engineered with these factors in mind, but still require careful programming for these special circumstances.
When used correctly, pacemakers and defibrillators improve both quality of life and life expectancy. While teams of engineers design these small machines, they rely on doctors knowing who will benefit from this technology and how to program the software to best serve each specific patient and scenario.